Introduction to Patellofemoral Pain Syndrome
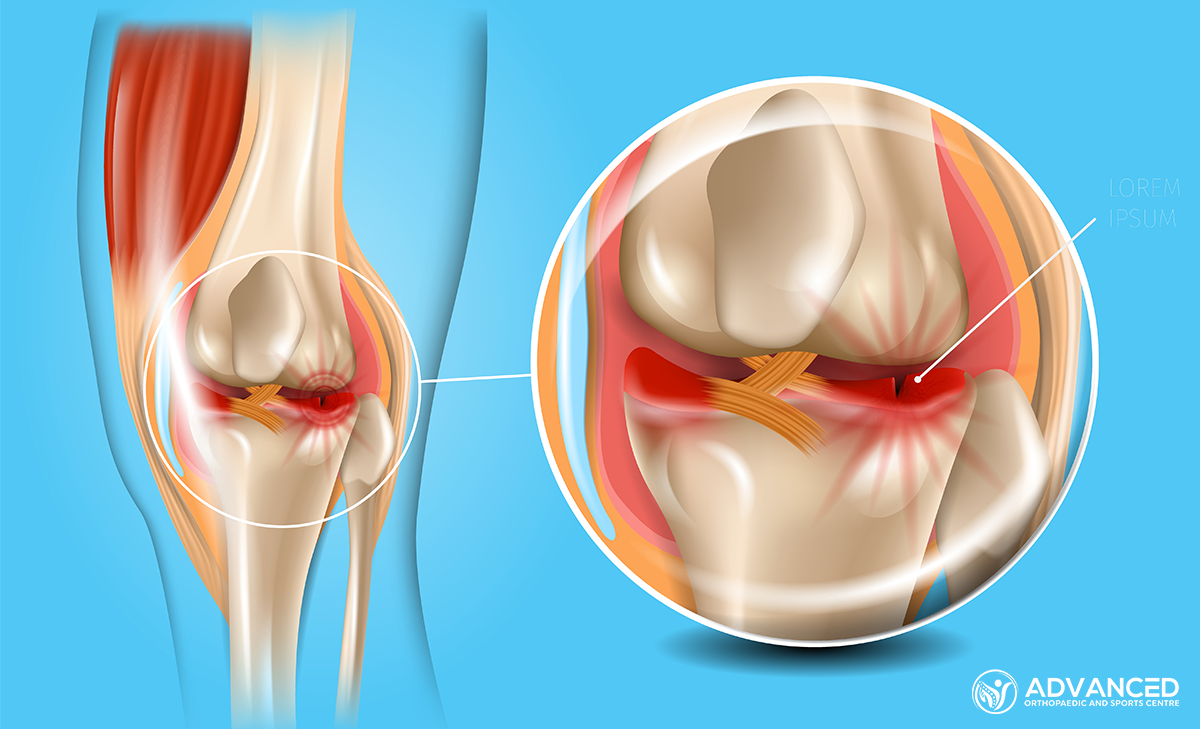
Patellofemoral Pain Syndrome (PFPS), often known as runner’s knee, is a condition that impacts the knee joint, especially among athletes and active people. It involves pain around or behind the patella (kneecap), where it articulates with the thigh bone (femur).
Despite its common occurrence, PFPS is effectively manageable. Understanding its causes, symptoms, and treatment options can help those affected return pain-free to their regular activities.
Causes of Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome (PFPS) results from various factors, not just one single issue. The main causes include:
Movement and Alignment Issues
- Knee Joint Misalignment: If the kneecap doesn’t move correctly over the thigh bone when you bend or straighten your knee, it can lead to uneven pressure and pain.
- Muscle Weakness: Weak thigh muscles, especially the inner part of the quadriceps, can cause the kneecap to move out of position.
- Foot Structure: Flat feet or feet that roll inwards too much can affect how your leg lines up with your knee, leading to PFPS.
Overuse and Activity-Related Factors
- Intense Training: A sudden increase in intensity or training can put too much stress on your knee.
- Repetitive Movements: Activities that involve a lot of knee bending, like running, jumping, or cycling, can put extra stress on the kneecap.
Other Factors
- Injury: A direct hit to the knee or past knee injuries can make you more likely to get PFPS.
- Age and Gender: It’s more common in young adults and women, possibly because of differences in body structure and hormones.
Symptoms and Diagnosis of PFPS
Identifying Patellofemoral Pain Syndrome (PFPS) involves recognising its distinctive symptoms and undergoing a detailed medical evaluation:
Symptoms of Patellofemoral Pain Syndrome
- Pain Around the Kneecap: This is often felt when sitting with bent knees, squatting, jumping, or using stairs.
- Popping or Grinding Sensations: Some people may experience these sensations in the knee during movement.
- Stiffness and Swelling: The knee may feel stiff or swollen after periods of inactivity or intense activity.
Diagnosing Patellofemoral Pain Syndrome
Diagnosing PFPS typically involves a thorough examination. The knee’s alignment, muscle strength, and movement patterns may be assessed to identify signs of PFPS.
Imaging tests like MRI or X-rays are seldom necessary but can be used to rule out other conditions. The diagnosis is mainly based on the patient’s symptoms and the physical exam findings.
Management and Treatment Options
The approach to managing Patellofemoral Pain Syndrome (PFPS) focuses on alleviating symptoms, improving knee function, and preventing future episodes. Treatment is often conservative, emphasising non-surgical methods. Here are the primary strategies employed:
Conservative Treatments
- Physical Therapy: Aims to strengthen the muscles around the knee, particularly the quadriceps, to improve patellar alignment and function.
- Activity Modification: Patients are advised to avoid high-impact exercises and gradually reintroduce activities as symptoms improve.
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce pain and inflammation. Ice therapy is also beneficial for managing acute pain and swelling.
Supportive Measures
- Orthotic Devices: For people with foot mechanics contributing to PFPS, orthotic insoles may help by correcting foot alignment and distributing pressure more evenly.
- Knee Braces or Taping: These can provide additional support and help maintain proper knee alignment during activities.
Advanced Treatments
In cases where conservative treatments do not lead to improvement, more advanced options may be considered:
- Injections: Corticosteroid injections around the knee can temporarily relieve inflammation and pain.
- Surgery: Rarely, if there is significant structural damage or misalignment, surgical intervention may be necessary to correct the underlying issues.
Rehabilitation and Physical Therapy
This phase is dedicated to restoring strength, flexibility, and proper function to the knee, aiming to alleviate pain and prevent recurrence. Key components of a rehabilitation program include:
Strengthening Exercises
- Quadriceps Strengthening: Focuses on the muscles at the front of the thigh to ensure the patella tracks correctly in its groove.
- Hip and Core Strengthening: Enhances stability of the pelvis and knee, reducing the risk of misalignment and uneven stress on the joint.
Flexibility and Stretching
- Hamstring and Calf Stretching: Tight muscles in the back of the thigh and calf can contribute to knee pain by altering gait and patellar alignment.
- Iliotibial Band Stretching: The iliotibial band runs along the outside of the thigh, and its tightness can exert additional pressure on the knee joint.
Proprioception and Balance Training
Improving proprioception (the body’s ability to perceive its position in space) and balance can help protect the knee from awkward movements and further injury.
Manual Therapy
Manual techniques such as massage and mobilisation may also be employed to improve knee movement and surrounding tissues.
Prevention Strategies
Preventing Patellofemoral Pain Syndrome (PFPS) involves addressing the factors contributing to its development. Strategies may include:
Proper Training and Exercise Techniques
- Gradual Increase in Activity: Avoid sudden spikes in exercise intensity or duration to minimise stress on the knee.
- Cross-Training: Incorporate various activities to distribute stress and prevent the overuse of specific muscle groups evenly.
Strength and Flexibility
- Regular Strengthening: Focus on the quadriceps, hips, and core muscles to improve stability and alignment of the knee joint.
- Flexibility Exercises: Stretch the hamstrings, calves, and iliotibial band regularly to maintain muscle balance and reduce tension on the knee.
Footwear and Orthotics
- Appropriate Footwear: Wear shoes that offer good support and are suitable for the specific activity to help maintain proper leg alignment and balance.
- Use of Orthotics: For those with foot structure issues contributing to PFPS, custom orthotic inserts can correct misalignments and distribute pressure more evenly.
Posture and Ergonomics
- Mindful Posture: Maintain awareness of knee positioning during daily activities and sports to avoid putting unnecessary stress on the patellofemoral joint.
- Ergonomic Adjustments: Ensure work and living environments support proper posture and do not encourage positions that may strain the knee.
Conclusion
Patellofemoral Pain Syndrome (PFPS) is a manageable condition that benefits from early diagnosis, targeted treatment, and consistent rehabilitation efforts. By understanding and addressing the multifaceted aspects of PFPS, people can achieve pain relief and return to their daily and athletic activities.