Introduction to Knee Rheumatoid Arthritis
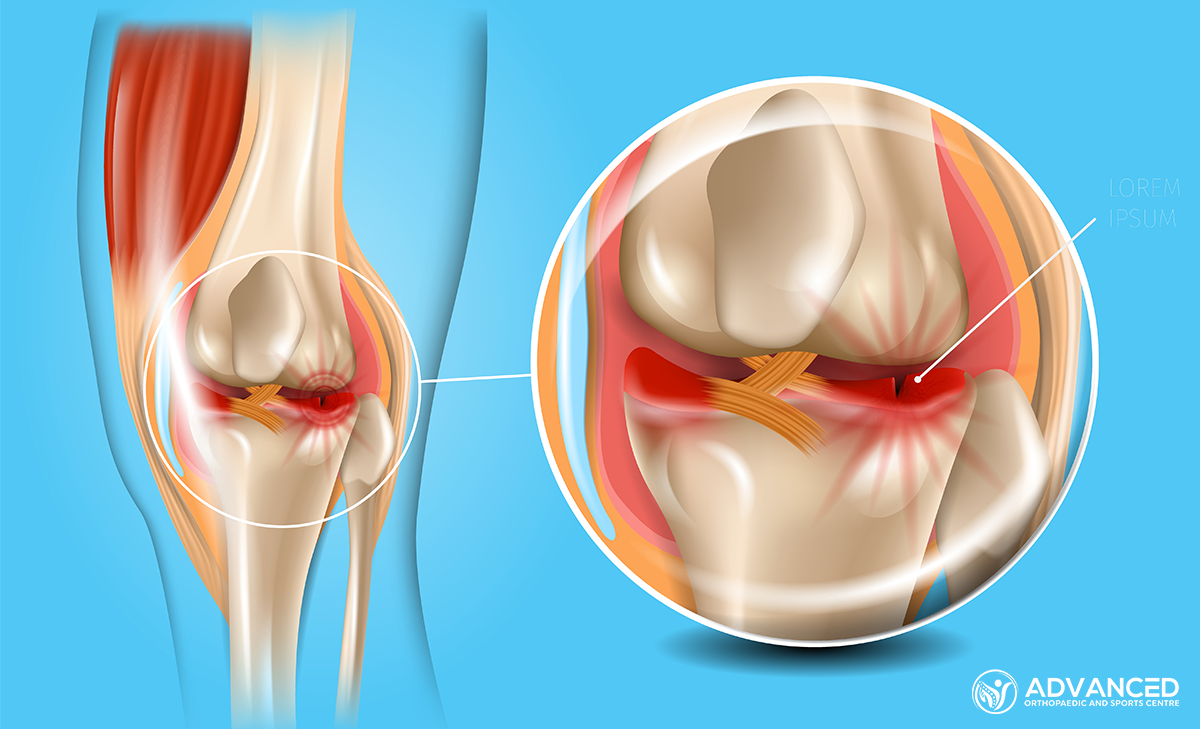
Knee Rheumatoid Arthritis (RA) is an autoimmune condition characterised by joint inflammation, which leads to pain, swelling, and reduced mobility. Unlike osteoarthritis, which results from wear and tear, RA involves the body’s immune system mistakenly attacking the joint lining.
This condition most commonly affects the hands, feet, and knees, causing varying degrees of discomfort and disability. Early diagnosis and treatment help manage symptoms and prevent long-term joint damage.
Causes and Risk Factors of Knee RA
Rheumatoid Arthritis (RA) in the knee arises from various genetic, environmental, and immunological factors. The exact cause of RA remains unknown, but it is understood to involve the immune system attacking the synovium, the lining of the membranes surrounding the joints. Risk factors for this condition include:
Genetic Predisposition
People with certain genetic markers are at a higher risk of developing RA, indicating a hereditary component to the disease.
Environmental Triggers
Exposure to environmental factors such as smoking, air pollution, and certain viruses may increase the risk of triggering RA in people with a genetic predisposition.
Hormonal Influences
Hormonal changes may also heighten the risk, with women being more prone to developing RA, suggesting that sex hormones could influence disease risk and progression.
Symptoms and Diagnosis
Symptoms
Rheumatoid Arthritis (RA) in the knee can manifest through a range of symptoms, which may vary from person to person. Key indicators include:
- Joint Pain: Pain in the knee joints is often a symptom of RA, worsened by movement or after periods of inactivity.
- Swelling and Warmth: The knee may appear swollen and feel warm to the touch due to inflammation.
- Stiffness: People may experience stiffness in the knee, especially in the morning or after sitting for long periods.
- Reduced Range of Motion: RA can lead to a decreased ability to move the knee through its full range of motion.
- Fatigue and General Discomfort: General feelings of fatigue are common, reflecting the systemic nature of the disease.
Diagnosis
Diagnosing Knee RA involves a combination of clinical evaluation and diagnostic tests. This typically starts with a medical history and physical examination, looking for common RA symptoms and assessing joint function.
Laboratory tests, such as blood tests for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, help confirm the presence of autoimmune processes. Imaging tests, including X-rays, MRI, and ultrasound, are used to visualise joint damage, inflammation, and the presence of synovial fluid.
These diagnostic tools collectively enable a comprehensive assessment, facilitating accurate diagnosis and tailored treatment planning.
Treatment Options for Knee Rheumatoid Arthritis
Treatment strategies are personalised, often involving a combination of the following:
Medications
Medications have several classes of drugs used to treat the condition:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can relieve pain and reduce inflammation. However, they do not prevent RA progression and may have side effects with long-term use.
- Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs (e.g. Methotrexate) slow or stop the immune system processes that trigger inflammation, helping to prevent joint and tissue damage.
- Biologic Agents: Biologic response modifiers, a subset of DMARDs, target specific steps in the inflammatory process.
- Corticosteroids: Corticosteroids can quickly reduce inflammation and pain, as well as slow joint damage, but are generally used for short-term relief
Physical Therapy
Physical therapy and braces or splints to support weakened joints can help improve mobility, strengthen muscles around the joints, and reduce overall pain levels.
Lifestyle Adjustments
Lifestyle changes, including maintaining a healthy weight, engaging in regular low-impact exercise, and eating a balanced diet, can help manage RA symptoms and improve overall health.
Surgical Options
In cases where medication and physical therapy do not sufficiently relieve symptoms or prevent joint damage, surgery may be considered. Surgical options range from synovectomy (removal of inflamed synovium) to joint replacement surgery.
Prevention and Management Strategies
While it’s not possible to completely prevent Rheumatoid Arthritis (RA) due to its unclear causes, specific strategies may help reduce the risk or mitigate the severity of symptoms:
- Avoid Smoking: Smoking is a known risk factor for RA and can worsen its severity. Quitting smoking can help lower this risk.
- Maintain a Healthy Weight: Excess weight puts additional stress on joints and can increase the risk of developing RA.
- Eat a Balanced Diet: A diet rich in antioxidants, omega-3 fatty acids, and fibres can help reduce inflammation and support overall health.
- Stay Physically Active: Regular exercise helps maintain joint flexibility and can improve overall health, potentially reducing the risk of RA.
- Monitor and Limit Alcohol Consumption: Excessive alcohol consumption can affect the risk of developing RA. Moderating alcohol intake is advised.
Conclusion
Managing Rheumatoid Arthritis (RA) effectively requires a well-planned approach to treatment and lifestyle adjustments. With appropriate medical care and lifestyle changes, people can maintain functionality and reduce the condition’s impact on their daily lives.